
New Techniques
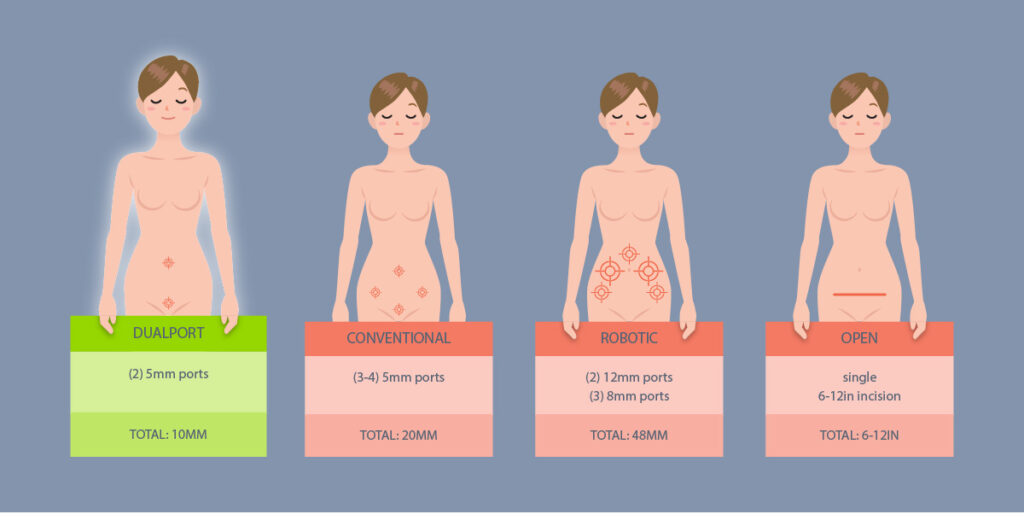
Today, 45% of women still undergo their mother or grandmother’s hysterectomy – which is an open procedure that can take 6 – 8 weeks for recovery. In addition, many women are now advised to have a GYN procedure with robotics, which offers no added benefits over standard laparoscopic procedures.
New advanced minimally invasive procedures make it possible for all GYN surgery to be performed with just two small incisions. This reduces the risk of complications, minimizes pain and recovery time, and improves overall outcomes for the patient. Keep reading to learn more about:
DualPortGYN – Minimally Invasive GYN Surgery for all GYN conditions
LAAM – Minimally Invasive GYN Surgery for Uterine Fibroids
Retroperitoneal Dissection – A technique that allows the surgeon to navigate the pelvic region more safely and significantly reduce complications during GYN surgery.
Uterine Ligation or Occlusion – Techniques that allows the surgeon to control blood loss and significantly reduce complications during GYN surgery
DualPortGYN
What is DualPortGYN?
DualPortGYN is a technique developed by the specialists at The Center for Innovative GYN Care that improves the overall outcome of minimally invasive GYN surgery. Women with complex conditions are able to have surgery with only two tiny incisions, no bigger than a paper cut – one at the belly button and one at the bikini line. While the incisions are small, complicated conditions like large fibroids, an enlarged uterus or pelvic adhesions can all be treated with DualPortGYN.
Using 2 additional advanced techniques, retroperitoneal dissection and uterine artery ligation, surgeons can map the entire pelvic cavity and control blood loss. Most surgeries are performed in under an hour, in an outpatient setting.
Important note for women: DualPortGYN does not use a power morcellator, an instrument that cuts up and removes large tissue during certain laparoscopic and robotic surgical procedures. In 2014, the Food and Drug Administration (FDA) issued a warning discouraging morcellator-aided GYN surgery because these instruments may spread uterine cancer during the procedure.
How does it work?
Surgeons place one incision that is 5 millimeters long (3/16th of an inch) at the belly button and put another of the same size on the bikini line. Since the incisions are in the mid-line, the risk of muscle injury and bleeding is greatly reduced. And, the incisions become essentially invisible one to two months after a procedure. Once the surgeons make these tiny incisions, DualPortGYN also uses two highly specialized techniques to remove large masses safely – often in under an hour:
- Retroperitoneal dissection (RDP): Originally developed to remove cancerous tissue, RPD gives the surgeon a clear view of the pelvic cavity by going beneath the peritoneum (membrane) that surrounds the pelvic organs. This allows surgeons to map the organs and arteries in the pelvis, much like a GPS system, reducing the length of the procedure and avoiding injury to the pelvic structures.
- Uterine Artery Litigation (UAL): This technique temporarily blocks blood flow in the uterine artery during surgery to control bleeding, one of the more common complications of GYN surgery. This is important because keeping blood loss to a minimum reduces complication rates and speeds recovery.
What conditions can be treated using DualPortGYN?
DualPortGYN can be used to remove fibroids and to treat endometriosis, pelvic masses, ovarian cysts, pelvic adhesions, cancer and pelvic organ prolapse.
What are the benefits of DualPortGYN?
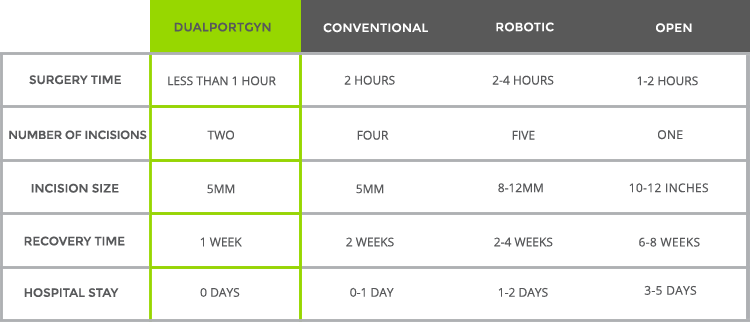
According to a comparison study of 400 hysterectomy procedures conducted by researchers at The Center for Innovative GYN Care in 2011, the DualPortGYN approach was shown to have the:
- Fastest recovery time
- Smallest incisions, and
- Lowest complications of any minimally invasive approach to surgery, including standard (conventional) and robotic approaches.
Despite new advances, approximately one-third of U.S. hospitals perform all hysterectomies through open surgery.
Unlike DualPortGYN, conventional laparoscopic and robotic approaches to surgery do not “map” the pelvis using the retroperitoneal approach, which means vital organs and arteries may not be identified in advance. This can increase the risk of injury, leading to higher complication rates and longer recovery times.
LAAM-BUAO
What is LAAM-BUAO?
LAAM-BUAO is a hybrid myomectomy technique. A myomectomy means removal of fibroids from the uterus while keeping the uterus in place, making it possible for women to get pregnant. Developed by surgeons at The Center for Innovative GYN Care to overcome the challenges and disadvantages of other myomectomy techniques, LAAM provides greater flexibility to effectively remove fibroids, despite their location, size or quanity.
Important note for women: LAAM does not use a power morcellator, an instrument that cuts up and removes large tissue during certain laparoscopic and robotic surgical procedures. In 2014, the Food and Drug Administration (FDA) issued a warning discouraging morcellator-aided GYN surgery because these instruments may spread uterine cancer during the procedure.
How does it work?
LAAM (Laparoscopic Assisted Abdominal Myomectomy) uses two small incisions, one at the belly button and one at the bikini line. It is specifically designed for women seeking fertility. Women who are past childbearing may not be candidates for LAAM. LAAM is not limited by fibroid size, number, or location. BUAO (Bilateral Uterine Artery Occlusion) is the blockage of the uterine artery during the procedure to control bleeding. Due to the advantage of the surgeon being able to feel all of the fibroids, LAAM is the most thorough minimally invasive technique used for a myomectomy. Most LAAM procedures are done in an outpatient setting, and patients are able to return to their lives sooner than with open procedures.
For fertility patients, Bilateral Uterine Artery Occlusion allows the surgeon to temporarily block blood flow during the surgery and then it is restored after the procedure is complete.
A LAAM surgery requires only two small incisions: a 5MM incision at the belly button, and a 1.5 inch incision at the bikini line. In general, the LAAM-BUAL procedure takes one hour (standard open procedures are up to four hours), can be performed as an outpatient procedure, and significantly reduces recovery time and surgical complications.
What are the benefits of LAAM-BUAO?
A successful myomectomy requires the surgeon to remove fibroids often deep in the muscle of the uterus that cannot be easily seen. It also requires the surgeon to remove all of the fibroids, including smaller ones, which can only be located by feel. Accordingly, LAAM allows the surgeon to feel all of the fibroids at any location in the uterus, and allows for their safe and effective removal no matter the size.
In comparison, standard and robotic laparoscopic approaches to myomectomy do not allow the surgeon to feel fibroids in the uterus. Without this sense of touch, surgeons can miss fibroids deep in the muscle, which can cause problems with infertility and persistent bleeding. In addition, LAAM is more convenient for women. Generally, the procedure can be performed in about an hour on an outpatient basis, with a shorter recovery time than other forms of myomectomy, and with less complications.
LAAM-BUAO Compared with Other Procedures Based on Size of the Fibroids

LAAM-BUAO Compared with Other Procedures Based on the Number of Fibroids
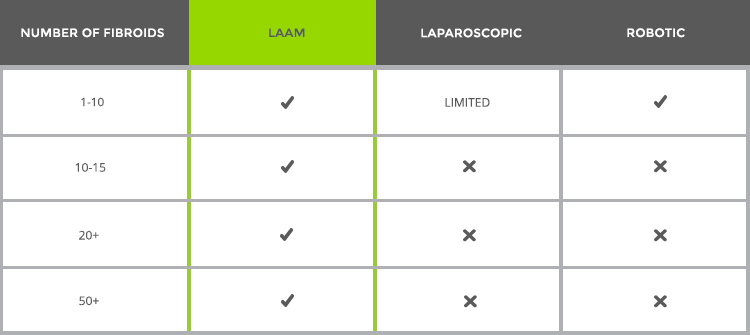
Overall Benefits of LAAM-BUAO Compared to Other Procedures

Retroperitoneal Dissection
What is Retroperitoneal Dissection?
Retroperitoneal dissection, or RPD for short, is an important technique in minimally invasive GYN surgery. RPD is a way for surgeons to go underneath a membrane in the abdominal cavity (called the peritoneum) that surrounds the pelvic organs. Surgeons can then have a clear view and can to “map” the entire area. This makes it possible to see the large blood vessels, the bladder and the ureter – the tube that transports urine from the kidney to the bladder – to avoid injuring these structures during GYN surgery.
Surgeons need special training to perform RPD. Currently, DualPortGYN and LAAM are the only laparoscopic techniques that routinely use retroperitoneal dissection in GYN surgery. RPD is used for hysterectomy, myomectomy, resection of endometriosis, ovarian cystectomy, resection of pelvic adhesions and prolapse repair.
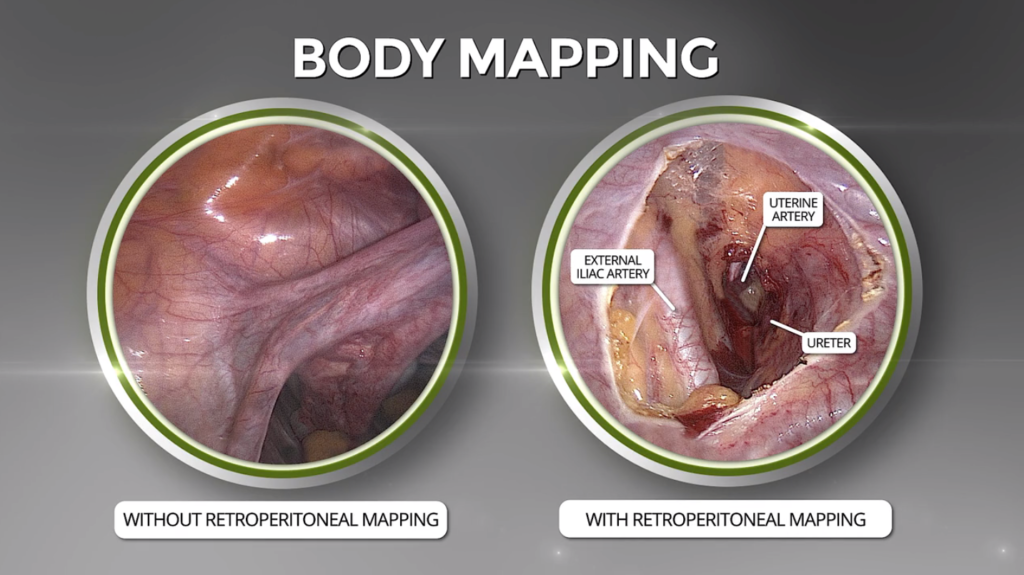
What are the benefits of Retroperitoneal Dissection?
RPD allows surgeons to map the organs and arteries in the pelvis, much like a GPS system. This avoids injury to the pelvic structures and makes it possible to perform minimally invasive laparoscopic surgeries quickly and with less blood loss, smaller incisions, and faster recovery times than with standard laparoscopic, robotic, or open surgical procedures. RPD can be used in removing fibroids and pelvic masses and in surgeries to treat endometriosis, prolapse, uterine cancer and other GYN conditions.
Benefits of RPD in Action
When women undergo GYN surgery, a potentially serious complication is injuring the ureter, a long tube about 10 to 12 inches long that carries urine from the kidney to the bladder. Since we have two kidneys, there are two ureters, one attached to each kidney. The upper half of the ureter is located in the abdomen and the lower half is located in the pelvic area.
However, in most situations, injuries typically occur to the ureter closest to the bladder when the ureter is not completely seen by the surgeon. When this happens, or the ureter’s location is unknown, the surgeon can inadvertently cut the ureter, place a clamp or suture on it (ligate), or cause other injuries. The result can be sickness, infection, permanent kidney damage or having to remove a kidney.
To prevent these complications, CIGC surgeons use a technique called ureterolysis, which frees the ureter from surrounding tissue so trained surgeons are able to move the ureter out of harm’s way. This requires the surgeon to be knowledgeable about the anatomy of the pelvic cavity and to be trained in using highly advanced surgical techniques.
Uterine Artery Ligation or Occlusion
What is Uterine Artery Ligation or Occlusion and what are the benefits?
Uterine artery ligation (permanently) or occlusion (temporarily) controls blood loss safely away from the ureter, which can often be damaged in laparoscopic surgery, including robotic surgery. In procedures where this technique isn’t used, it is often necessary to have additional surgery to repair damaged ureters. Ligation is used for hysterectomy, and for myomectomy for women who wish to retain their uterus, but no longer wish to have children. Occlusion is used for myomectomy for women who still wish to be able to conceive a child.


